Renal Transplant
Remote kidney clinic heralds a homecoming for Aboriginal patients after years spent away
Barbara Reid wishes she could have been there for those important early moments in her granddaughter's young life
— her first steps, first words and big smile...

Kidney Transplant Rates For Aboriginal Australians
Data released by Kidney Health Australia in December 2017 showed:
- Indigenous patients are 10 times less likely than non-Indigenous patients to be added to the waiting list for a kidney donation transplant.
- About 13% of patients receiving dialysis treatment in Australia are Indigenous. Only 241 of 10,551 patients with a functioning kidney transplant are Indigenous.
- According to Kidney Health Australia, about 30 of 800 kidney transplants performed each year are received by Indigenous Australians.
Indigenous Health Minister Ken Wyatt said he was disheartened with the figures and wants to focus on building a heightened awareness of the issue. This under-representation can be attributed to a variety of reasons such as comorbidities, delays in listing and significant tissue matching issues as well as some structural racism. Importantly, the outcomes from transplantation are considerable poorer than among non-Indigenous people.
To improve access to transplantation by Aboriginal and Torres Strait Islander renal patients, there needs to be a better understanding of how to address the barriers. There also needs to be improved support services for patients.
The reasons for poor access to transplantation experienced by Aboriginal and Torres Strait Islander Australians are complex and can be attributed to:
- The greater burden of comorbid illness amongst Aboriginal and Torres Strait Islander dialysis patients leading to fewer patients being judge medically suitable;
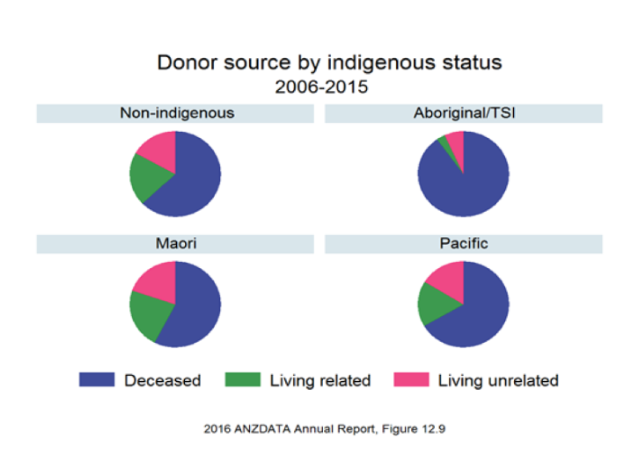
- The shortage of living and deceased donors from within Aboriginal and Torres Strait Islander communities;
- The length of time on the waiting list and matching system;
- The challenges in delivering appropriate health services to people living in remote areas who might also have low health literacy and not speak English as a first language;
- The dislocation that follows from moving to transplant centres in distant capital cities; and
- The high complication rate, particularly in terms of early infectious complications leading to poor transplant outcomes, including substantially higher death and graft loss rates.
The poorer outcomes among Indigenous people who receive transplants are due to higher rates of rejection, less well-matched kidneys, higher rates of infection and infection-related deaths.
Poor access to transplantation can also result from the requirement for significant work up tests and assessments which require visits to major centres. After transplantation there is the prospect of a post-operative stay and side effects away from home and supports.
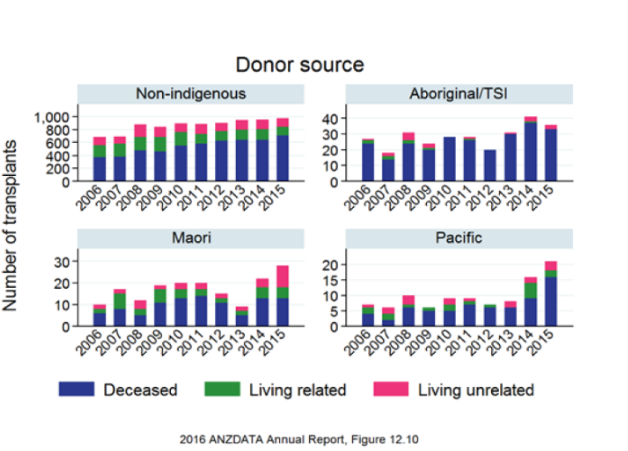
Kidney Transplant Donor Source
Number of Kidney Transplants